
The purpose of the information you will find on our website is to help you and your partner get to know the practical side of the Assisted Reproductive Technology (ART) program, so that you can prepare and organize in a timely manner.
CCAR’s highly educated staff offers each couple an individual treatment tailored to their special needs.
Our team consists of specialists from all fields of reproductive medicine, providing our patients with the most modern methods in the field of assisted reproduction in a space that is specially designed to ensure the best outcome, that is, the birth of a healthy baby. Codra Center for Assisted Reproduction (CCAR) is the largest center of this type in Montenegro.
We hope that the information from our site will be a source of useful information and will bring you closer to the different types of treatment that CCAR can offer. Please feel free to contact our professional staff for any clarifications and possible doubts. Our reception is located on the ground floor of the first building (Codra I). When you arrive, please bring your ID card with you, state the name of your consultant and the agreed appointment.
General information
Assisted fertilization techniques are used only when there is no other possibility of reproduction. Our first step in treatment is consultation and counseling.
Before starting any treatment, various examinations need to be done and it may take some time, before starting the procedure.
In order to protect babies born through the procedure of assisted reproduction, couples who enter the procedure are tested for various diseases, and you may be subjected to additional, special tests.
Blood tests and ultrasound examinations will be performed during the treatment.
It is preferable to avoid intercourse without protection, from the beginning of the treatment. It is also advised that the husband/partner abstains for 2-3 days before the scheduled aspiration.
General health information
Smoking reduces the possibility of conception, regardless of whether it is a woman or her partner. We advise you to stop smoking at least 2-3 months before the start of the procedure, in order to increase the chances of success.
Body weight: The percentage of conception is lower in women with increased body weight, compared to women who are of normal body mass. You can get advice and a program for body mass correction from our endocrinologist.
Also, in “fuller” men, the number and quality of spermatozoa can be significantly reduced.
Neural tube defect: (spina bifida) : to reduce the risk of spina bifida in the baby, we advise you to take 400mg of folic acid daily.
Note: Many staff members are involved in your treatment. You will meet some of them during your visits to CCAR, while others are “behind the scenes”. If there is anything you do not understand, please ask us. But since the treatment is tailored to each couple individually, don’t be surprised if other couples have a different treatment. If in any segment of the cycle things do not go according to plan, your procedure may be suspended.
Intrauterine insemination (IUI, AIH, IUTPI)
It involves introducing a specially prepared suspension of (wife/partner’s) sperm into the woman’s uterus, with the help of a soft catheter that has previously passed through the cervix. The fundamental prerequisite for this procedure is primarily the patible fallopian tubes. The most common indications for insemination are: reduced male fertility, unfavorable quality of cervical mucus or the presence of anti-sperm antibodies, as well as unknown causes of sterility.
Insemination (IUI/AIH) can be carried out in a natural or stimulated cycle.
NEW: In our Center, a new method of insemination is available – IUTPI, which, compared to the classic IUI method, increases the percentage of pregnancies achieved by 20%.

If insemination is not the method of choice in your case, or you have already done it several times without a successful outcome (usually, a maximum of three times), we will suggest you to approach one of the two methods of in vitro fertilization. What these methods have in common is that they both start with an egg aspiration procedure, which can be performed both in a stimulated and in a spontaneous cycle.
How is an IVF procedure performed?
In Vitro Fertilization (IVF) is the medical term for “test tube baby”, which means that, due to the impossibility of the said process taking place spontaneously in the body, egg cells and spermatozoa are joined in laboratory conditions.
Each IVF treatment consists of several stages:
Down-regulation or inactivation of egg production in the ovary
Stimulation of egg production
Ultrasound monitoring-monitoring of growth and development of follicles, with blood analyses
“Stop injection”
Aspiration
Fertilization of eggs and monitoring of embryo development
Embryo-transfer and/or freezing of high-quality embryos
Luteal phase support
After the phase of inactivation of egg production, the gynecologist determines the beginning of the phase of hormonal stimulation of the ovaries, so that your follicles begin to grow and produce eggs.
MONITORING OF FOLLICLE DEVELOPMENT
As the follicles grow, they produce the female hormone estrogen. The level of estrogen produced in the follicles is periodically measured during treatment. The level of estrogen is important for measuring the response of your ovaries to the applied hormone therapy – stimulation, as well as for the detection of hyperstimulation (see – OHSS). Follicle growth can also be measured by vaginal ultrasound to determine the number of follicles, assess their size and characteristics, and determine the thickness and quality of the endometrium.
By combining the results of the estrogen level and the ultrasound examination, the ideal time for aspiration is decided. The time of aspiration is controlled by giving a so-called “stop injection”, i.e., an injection of human chorionic gonadotropin, which is given 36-38 hours before the start of aspiration, i.e. when, based on an ultrasound examination, it is established that there are 3 or more follicles with a diameter of 18 mm.
So, after successfully performed hormonal stimulation, at the exact agreed time, you will receive the so-called “stop injection”, after which we will start the VTO procedure by aspiration of your eggs.
OAG ASPIRATION
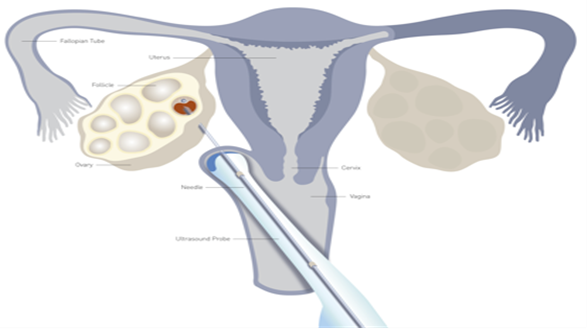
Before starting the aspiration, you will receive intravenous anesthesia, or a strong analgesic, or a sedative. Aspiration is performed in the hall of the IVF department (located right next to the embryology laboratory) by specially trained doctors. An essential condition for puncture is a completely empty bladder. The intervention is performed transvaginally, under ultrasound control. A special puncture needle, which is connected by a catheter system to vessels for collecting suctioned contents, pierces the vaginal wall and enters the ovary. After piercing the follicle, the liquid containing the egg cells is aspired. The injection is not too painful and patients who opt for the intervention without general anesthesia usually tolerate it well. Containers for collecting the aspirated content were previously prepared and heated to body temperature. The embryologist immediately examines the submitted material under a microscope and announces the number of oocytes obtained. The resulting oocytes are then washed and placed in a culture medium. It is important to know that not all follicles must contain an ovum. Follicle puncture and oocyte aspiration is a step in the assisted reproduction procedure that can end in failure and require abandonment of the procedure. Some of the reasons for egg failure are known, but not all. The most common cases are:
when follicles containing mature eggs do not develop in the cycle;
when natural ovulation occurs before oocyte puncture;
when, for various reasons, it is not possible to access the egg cells, or some other technical difficulties occur that prevent the puncture of the same.
The procedure lasts an average of 5-15 minutes, depending on the number of follicles. After the intervention, you will stay in our hospital for another hour or two to rest, until you are approved to go home. Before you go home, you will receive an interim report on all the essential elements of the intervention. There will also be instructions on the therapy that will be carried out until the moment when the best embryos will be returned to you (embryo transfer).
Addendum: On the day of the scheduled aspiration, the staff of the andrology laboratory will also prepare/process your husband’s/partner’s sample, for the needs of the VTO procedure.
STAGE OF SEED SAMPLE COLLECTION AND PROCESSING
The partner will provide a semen sample on the day of the oocyte puncture, at the agreed time. In order for the quality of the semen to be as good as possible, 2-3 days before the follicle puncture and egg aspiration, refrain from sexual intercourse. Seed preparation for the VTO procedure is done in the laboratory. On the day of follicle puncture and egg aspiration, you must submit the material for fertilization at the exact time agreed upon. It is best to give the sample in the apartment of our hospital, where you and your wife/partner will be accommodated. Beforehand, the responsible nurse will provide you with a sterile container and hand you a form, which you need to read first and then fill out. For practical reasons, before giving a sample, we advise you to:
– first wash your hands well
– carefully open the sterile container and place the lid in the foil that the container was covered with
– do not touch the inside of the container and the lid
– close the container with the sample carefully and well after you have finished giving the sample
– if you give the sample at home, try to keep it at body temperature (best next to the body) until you hand it over to the laboratory
The nurse in charge will take over and adequately mark your material, and then take it to the laboratory with the accompanying sheet you filled out. In rare cases, we may ask you for another sample, so your presence is required until you receive information from the laboratory that everything is in order.
VTO methods
Conventional IVF
The conventional IVF method is designed to help women with damaged fallopian tubes, in such a way that the egg cells collected by aspiration are prepared for insemination, that is, the addition of processed seminal fluid of the husband/partner to the medium in which the mentioned egg cells are already found. In this way, the spermatozoa are given the opportunity to find their way to the egg cells and fertilize them. However, in order for conventional IVF to be considered as a potential treatment for infertility, it is necessary that the spermogram of your husband/partner has all normal parameters.
Unsuccessful fertilization after IVF
In rare cases, unfortunately, fertilization does not occur, despite the “normal” appearance of eggs and sperm. The most common cause is the inability of the sperm to break through the barriers around the egg cell, although the eventual failure can also be related to the quality of the egg cells themselves.
It should also be borne in mind that the quality of semen changes over time, so the same man can unexpectedly produce poor quality sperm.
In cases of severe sterili
aunt of the man, the couple will be informed to consider the possibility of applying the method of micro fertilization (ICSI). In the most severe cases of complete absence of spermatozoa in the ejaculate (azoospermia), surgical sperm retrieval procedures can also be used: Micro-TESE, TESE, TESA, MESA, PESA (see: TREATMENT OF MALE INFERTILITY)
NEW: Only in our hospital is the Micro-TESE procedure available to you, which is performed by experts in the field of urology.

Intracytoplasmic sperm injection
As we have already mentioned, the cause of unsuccessful fertilization using the conventional IVF method can be the inability of spermatozoa to penetrate through the outer barrier (zona pellucida) or through the inner layer (vitelline membrane) of the egg cell. During the ICSI procedure, one spermatozoon is directly applied to the cytoplasm of the egg cell under the control of the microscope system and thus passes through both of these layers, which makes it possible to avoid the mentioned problem. The ICSI procedure is used in all couples with a reduced number and quality of spermatozoa, immature spermatozoa from the testicles or epididymis, in which the risk of unsuccessful fertilization is increased. This procedure is also applied to couples with previously unsuccessful fertilization, as well as in some cases of female sterility. The success rate varies depending on the type of problem.
NEW: At the Codra Center for Assisted Reproduction, the PICSI method is available to you, thanks to which we are able to extract and use mature, high-quality spermatozoa, which will improve the quality of your embryos, as well as their implantation potential.
We also offer our patients the possibility of physiological activation of spermatozoa, which will enable immobile spermatozoa to move, which is extremely important for patients who have a problem with the so-called. of immotile (immotile) spermatozoa, as well as the HOST method (Hypo Osmotic Swelling Test) when, among immotile (immotile) spermatozoa, it is necessary to separate live spermatozoa for injection.
Fertilization failure after ICSI
In some cases of male sterility, spermatozoa lack components that are very important for activation, and consequently for egg fertilization, which is actually the biggest cause of unsuccessful fertilization, which can sometimes happen even after ICSI.
With this method, as with conventional IVF, unsuccessful fertilization can also be related to the quality of the eggs.
NEW: In these situations, in our CCAR, we offer you the possibility of artificial egg activation, which will increase the chances of a successful outcome of the procedure.

(Intracytoplasmic Sperm Injection ICSI)
TREATMENT OF MALE INFERTILITY: In some men, spermatozoa are not present in the ejaculate (azoospermia). In such situations, the surgical retrieval of spermatozoa from the tissue of the testis or epididymis is approached.
NEW!!! Micro-TESE
In men who do not have sperm in the ejaculate, one of the options can be micro-TESE, microdissection of the testicular tissue. This procedure is performed under general anesthesia, in the operating room and with the help of a microscope and is only available to you in our hospital. The Micro-TESE method significantly increased the success rate of finding sperm in men with azoospermia. And what is especially important is that this procedure is much safer and less invasive for the patient, compared to other procedures, because the damage to the testicular tissue is minimal.
Testicular tissue biopsy (TESE)
Except in cases of complete absence of spermatozoa in the ejaculate, TESE can also be performed in men with an extremely low sperm count. Testicular tissue is taken from the testicles by open surgical biopsy and the spermatozoa thus obtained are used for the ICSI procedure.
Microsurgical aspiration of spermatozoa from the testes or epididymis (TESA/MESA/PESA)
These techniques are used when there is normal sperm production in the testes, but it cannot reach the seminal fluid (obstructive azoospermia). The vas deferens may be damaged or absent. Sperm can be aspirated directly from the testis (TESA) or from the epididymis (MESA, PESA).
Treatment of retrograde ejaculation
In certain cases of male sterility, the semen ends up in the bladder (retrograde ejaculation). In this case, in our hospital, a procedure is carried out by which, in a very simple way, it is possible to successfully isolate vital spermatozoa from urine and use them for the ICSI procedure.
This can happen in patients with diabetes, with neurological problems and in some patients after surgery.
Embryo Transfer (ET)
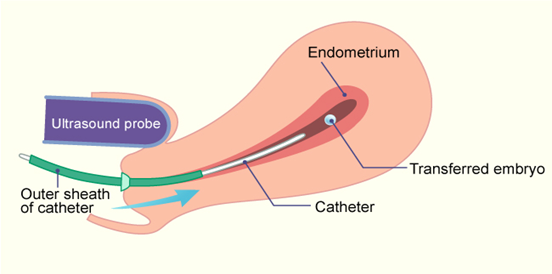
Embryo transfer (ET) is a painless procedure that does not require anesthesia and represents the crown of the VTO procedure. The best results are achieved if ET is performed under ultrasound control, where it is necessary that your bladder is full. Lying down after the transfer is not necessary. However, we advise you not to do anything strenuous and to refrain from sexual intercourse until you know the outcome of the procedure.
If more embryos are returned, the chances of pregnancy are higher, although the frequency of multiple pregnancies also increases. The number of returned embryos is determined on an individual basis and a maximum of 3 can be returned. All high-quality embryos that remain after ET can be vitrified (frozen) at your request and stored for a subsequent cycle, which will save you from going through the procedure again. .
No special preparation is required on your part for the embryo retrieval procedure (you will receive all the information in writing). Immediately after the intervention, there is no reason to lie down for more than 15 minutes. You will receive a discharge list, which you must carefully study, especially the part about the proposed therapy.
AFTER EMBRYOTRANSFER: (ET)
Limit intensive activities for the first few days. This does not mean that you have to lie down, but that you do not exert yourself physically. Read, walk, etc.
When bathing, avoid lying in the bathtub, use the shower
Do not use tampons
Refrain from intimate relations until the pregnancy test
Do not engage in heavy physical work
You can return to your usual activities a few days after the embryo transfer.
Fifteen days after the embryo transfer, a test should be done to prove early pregnancy – beta-hCG hormone from the blood, specific for pregnancy. A positive test is proof of the so-called biochemical pregnancies. It’s still not a real pregnancy, but there is still reason to be happy. Definitive confirmation of the existence of pregnancy is performed by an ultrasound examination. This examination is usually scheduled one month after the embryo transfer. A negative test, especially if bleeding has not occurred, still does not mean that the fertilization attempt has failed, although the chances of a favorable outcome are small. In such a situation, Utrogestan therapy should be continued and the test repeated in 3 to 4 days. If the result is negative again, the therapy is stopped. If the procedure was unsuccessful and you have a cycle, please also inform us about this, so that we can plan the next step.
COMPLICATIONS IN VTO
Ovarian Hyperstimulation (OHSS)
Ovarian hyperstimulation is very rare, but unfortunately, sometimes a possible complication. It is characterized by the enlargement of the ovaries, which causes discomfort, pain and accumulation of fluid in the abdomen and around the lungs. Some women feel nauseous, vomit, their abdomen is enlarged, they have difficulty breathing, which requires hospitalization.
If you show an excessive response, it may be necessary to stop the cycle or stop the FSH injections, followed by a stop injection. In these situations, it may be necessary for the resulting embryos to be vitrified (frozen) and returned in a subsequent, natural cycle.
Repeated unsuccessful implantation attempts and patients with miscarriages
Growth factors are normally found in high concentration in the female reproductive tract where they support the development of the embryo, its implantation and the development of the placenta.
In cases of repeated, unexplained, unsuccessful implantations, in patients with miscarriages, in smokers, etc., growth factors are present in a lower concentration or are absent at all.
NEW: In that case, CCAR offers you and enables the cultivation of embryos in a special medium, based on growth factors, which are naturally present in the female reproductive tract, which enables an increase in the number of embryonic cells, i.e. improves the development and quality of your embryos. In addition, in our Center for Assisted Reproduction, we can perform the so-called “priming” of the endometrium. More precisely, with the help of a special medium, we will prepare your endometrium for the best possible acceptance of embryos, thereby increasing the chances of their implantation.
EMBRYO FREEZING PHASE
During IVF treatment, there is a real possibility of obtaining more viable embryos than it is desirable to obtain for embryo transfer. Although we prefer a “single” embryo transfer, experience has shown that optimal chances of conception, with an acceptable risk of multiple pregnancy, is provided by the transfer of 2 to 3 embryos, depending on the age of the patient and the quality of the embryos.
If, as a result of the fertilization procedure, we have more than three viable embryos, our center offers you the possibility that the surplus of viable embryos (embryos of suitable quality) remaining after the embryo transfer, be preserved for future use by the process of controlled freezing (slow-freezing or vitrification) and thawing. In CCAR, embryos are frozen using the vitrification process (quick freezing), which increases the degree of survival of the embryos, but also the possibility of pregnancy after thawing.
IMPORTANT TO KNOW:
not all newly obtained embryos are of suitable quality to be suitable for the procedure of controlled freezing and thawing. Accordingly, we are unable to offer all our patients the option of vitrification (freezing) of embryos;
some or all embryos may not survive the freezing and thawing process
PHASE OF SPERM FREEZING
Sperm can also be frozen and stored for future use in insemination or IVF programs. Spermatozoa stored in this way can be used as a reserve, in cases where there is doubt about the ability to produce quality sperm in the future, i.e. vital spermatozoa. Some of the reasons to consider sperm freezing are:
– before therapy that would threaten the vitality of spermatozoa (cancer);
– before ligation of the vas deferens;
During diagnostic testicular biopsies (TESA, TESE, MicroTESE), it is wise to freeze part of the material to avoid reoperation. The material thus obtained can only be used for the ICSI procedure.
VTO success rate
The success rate of VTO varies depending on: the cause of sterility, the duration of sterility, the age of the woman, the body weight of the woman and man, the number and quality of the obtained eggs, spermatozoa and embryos returned. In general, 40-50% of couples achieve pregnancy, while 30-40% of couples will have a baby. The overall success rate after the third attempt is around 70-80%.
The miscarriage rate is the same as with spontaneous conception naturally.
HOW TO INCREASE THE OPPORTUNITIES FOR SUCCESS VTO
Although medical science does not currently recognize any factor that could adversely affect the success of assisted reproduction, we still advise you the following:
For women:
Avoid medications, except as prescribed. If you are taking your regular therapy, consult your gynecologist before entering the IVF cycle.
Do not smoke and avoid drinking alcohol. Studies prove that smoking and drinking alcohol can result in a lower success rate and a higher risk of miscarriage.
Do not take more than 2 caffeinated beverages per day (coffee, tea).
Refrain from intercourse 2 to 4 days before egg aspiration and after the embryo transfer is completed, until it is determined whether pregnancy has occurred;
For men:
A temperature higher than 38° C can adversely affect the quality of the semen, therefore, avoid hot baths and saunas
Avoid consumption of alcohol and cigarettes
Refrain from intercourse for 2 to 4 days, but no more than 7 days before the puncture of your partner’s ovaries, that is, giving a semen sample for the laboratory.
In addition to all of the above, in our CCAR you can perform an analysis every day, with which the examination of marital infertility usually begins:
SPERMOGRAM
Instructions for providing a sample
In order to provide the best possible sample, it is recommended that you refrain from sexual intercourse (ejaculation) 2 – 3 days before the analysis (minimum 2, maximum 5 days).
You must NOT use any lubricants or condoms, as they may affect the quality of the sample.
The sample must be ejaculated directly into a sterile container, which you will receive in our hospital. It is very important that the complete sample is in the container. If this is not the case, please note this on the questionnaire, which you will be given to fill out.
When you finish ejaculating, carefully put the lid on and close the container well.
You can also give the sample at home, but it will probably take longer than 30 minutes (the sample should be submitted for analysis, no longer than 30 minutes after ejaculation). For this reason, it is preferable that you give the sample in our hospital, where private apartments are provided for you.
If you still decide to give the sample at home, after ejaculation, put the container with the sample in a dark bag to protect it from light and, if possible, transport it to the hospital immediately, making sure that the sample maintains its temperature until then.
In order for us to be able to analyze your sample, it must be marked with your personal data. That’s why we ask you to bring your ID card with you and fill out the questionnaire, which you will also receive at our reception. Don’t forget to write down the time the sample was given, as well as the number of days of abstinence.
You can schedule this analysis by calling the phone numbers of our CALL center: +382 20 / 648 – 334; 648-335; 069 300 300 or tell your doctor to make an appointment. You can also contact the same phone numbers if you have any questions.
It takes at least 2 hours to make a spermogram, including morphology, after which you can come and collect your results.
SOON:
In addition to the above procedures, in order to provide the most complete and best service to all our patients, the Codra Center for Assisted Reproduction is preparing numerous novelties.
We hope that you have found useful information on our site. For any doubts or additional questions, feel free to contact us every working day or even better, to schedule your consultation appointment. The large expert team of the Codra Center for Assisted Reproduction will work on your problem with utmost responsibility and dedication. In addition, we will do everything to make you feel comfortable during your stay in our center.
With a great desire to help you on your way to parenthood and provide unreserved support, we are waiting for you…
Good luck!



